The 5 Rights of Cleaning and Disinfection
With healthcare-associated infection rates and multidrug-resistant organisms on the rise, and new pathogens emerging, a robust environmental cleaning and disinfection program is more important today than ever before. This article outlines a framework that can help healthcare facilities establish their cleaning and disinfection program, called the 5 Rights of Cleaning & Disinfection. The 5 Rights of Cleaning & Disinfection is a concept based on the nursing professions 5 Rights of Medication Administration. The 5 Rights include the:
- Right Products
- Right Locations
- Right People
- Right Moments
- Right Application
#1 — Right Products: A clean and sanitary environment is key to patient safety. In fact, it’s a requirement to participate in the Centers for Medicare and Medicaid Services (CMS) programs.1 CMS requires the use of EPA-registered hospital-grade disinfectants.2 While you will likely never see this language on a product label, a hospital-grade disinfectant must have kill claims for Staphylococcus aureus and Pseudomonas aeruginosa at a minimum.3 When selecting disinfectants, consider the pathogens of interest in the facility as well as the ideal properties which include:4
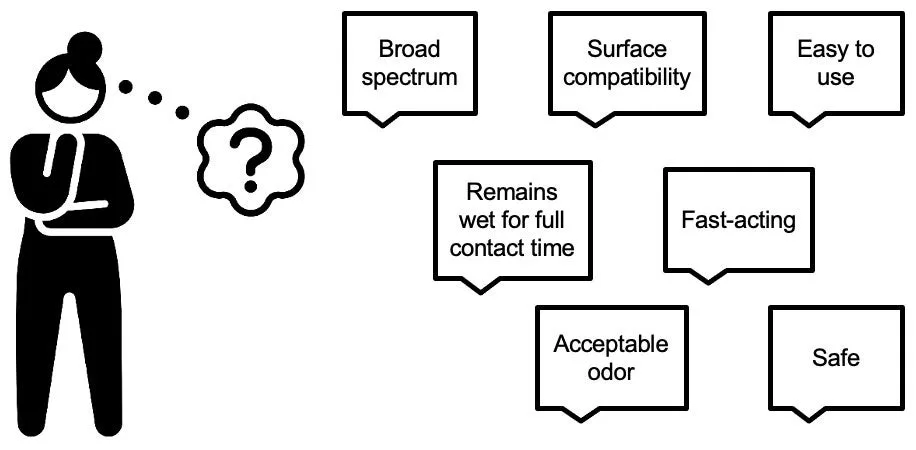
Reference: Rutala et al. (2014). Selection of the Ideal Disinfectant. ICHE; Vol 35(7)
Be sure to include stakeholders in the decision-making process such as the facility infection preventionist, environmental services (EVS) leadership and frontline workers, biomedical staff, facility safety officer, supply chain, and finance.
#2 — Right Location: Hospitals are complex communities, like small cities. There are many different areas in the hospital and cleaning and disinfection needs may differ based on transmission risks. With the current staffing challenges, certain areas might have to be deprioritized – such as office spaces. In fact, some facilities are having office staff clean their own spaces during this challenging time.
Another important element of Right Location are protocols. Ideally, there should be a protocol for each location in the hospital that addresses things like which product to use, the frequency of cleaning, and any nuances unique to that space.
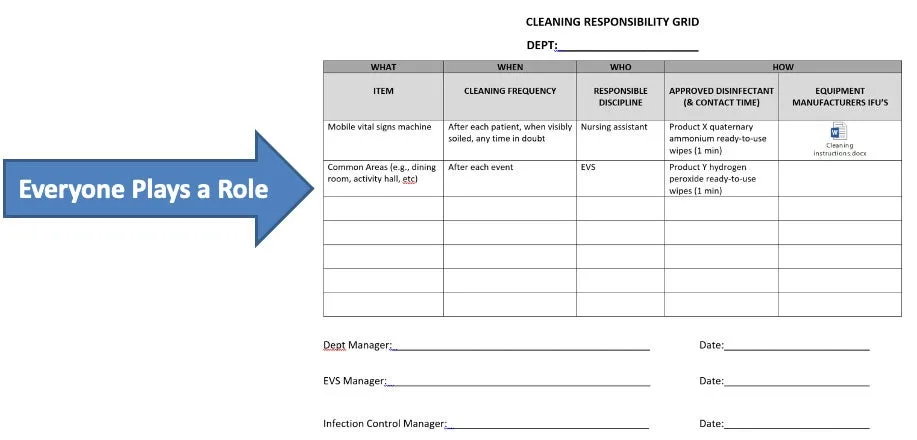
#3 — Right People: While EVS has primary responsibility to ensure a clean environment, everyone plays a role. Just like no healthcare workers are exempt from performing hand hygiene, no one should be exempt from performing cleaning and disinfection tasks. Non-EVS staff should clean and disinfect the non-critical equipment that they use – especially mobile equipment. They should also clean and disinfect high-touch surfaces in their work spaces at least once per shift. Nursing staff need to understand that for patient safety reasons, EVS does not clean equipment that is in use – at least they should not. Nursing staff really should be disinfecting the high-touch surfaces of this equipment like control panels, knobs & dials, handles and so on at least once per shift. Responsibility grids, like the example shown here, are a great way to communicate roles and responsibilities as it pertains to cleaning and disinfection.
#4 - Right Moments: Includes cleaning frequencies. In general, the guidance from the Centers for Disease Control and Prevention (CDC) states that cleaning should be performed in patient care areas at least once daily.5 However, there was no data to back this recommendation. But with the volume of foot traffic in facilities and patient rooms, is once a day really enough? Especially for touchable surfaces. In fact a 2015 study showed that it only took 4 hours for a surrogate virus to spread from HCW hands to almost half of the surfaces in a facility. The right frequency of cleaning should be targeted based on contamination events such as equipment that has been used with a patient or a bedside table before a patient eats.6
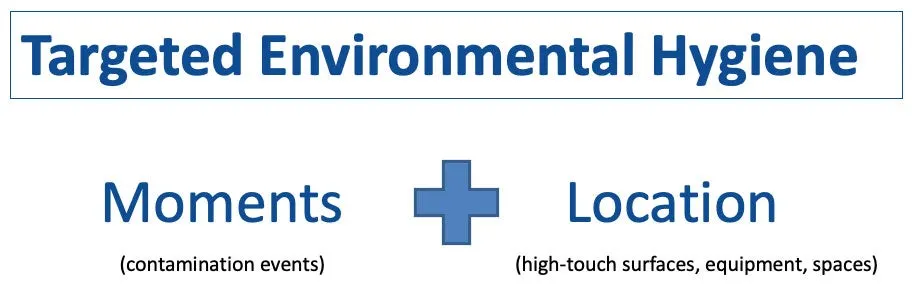
Some of the specific moments to consider increasing the frequency of cleaning and disinfection include when a facility is seeing an uptick in cases, during seasonal outbreaks, and of course, during epidemics or pandemics such as the current COVID-19 pandemic.
Additionally, the ideal time of the day for performing cleaning and disinfection should be determined. For example, some areas are more amenable to after-hours cleaning such as waiting rooms and other public spaces, operating rooms, and physician offices.
A final and very important moment is after equipment use – particularly portable or mobile equipment. Several outbreaks of Candida auris have linked such equipment as a source.
#5 — Right Application: Consider the most appropriate format of the product for the situation. Format types include ready-to-use wipes, spray bottles, pull-tops, and dilutables for example. Just like we have hand sanitizer available at every patient room, we should also have disinfecting wipes readily available for clinical staff.
The Right Application means that the product directions for use are followed – it’s the law! These include contact time and personal protective equipment. Cleaning should be methodical such as cleaning in a clockwise pattern around the room, from high surfaces to lower surfaces, and from clean to dirty.
Use of no-touch disinfection technologies like UV-C or electrostatic devices exploded during the pandemic. For areas where we may not have the resources to manually clean and disinfect as often or as thoroughly as we would like – such as waiting rooms and office spaces – use of these technologies could at least get us closer to the ideal.
Wrap-Up
A robust cleaning and disinfection program is critical to reducing the risk of infection transmission. The 5 Rights of Cleaning and Disinfection format will help you to think through what is needed in establishing such a program.
For a video walkthrough of the 5 Rights of Cleaning and Disinfection, please visit here.
References
^1. Centers for Medicare and Medicaid Services. State Operations Manual Appendix A, 2018. [Internet]. [Cited 2021 Dec 29]. Available from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_a_hospitals.pdf
2. Centers for Medicare and Medicaid Services. Hospital Infection Control Worksheet. [Internet]. [Cited 2021 Sep 20]. Available from https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertificationgeninfo/downloads/survey-and-cert-letter-15-12-attachment-1.pdf
3. Environmental Protection Agency. Antimicrobial Performance Evaluation Program [Internet]. [Cited 2021 Sep 20]. Available from https://www.epa.gov/pesticide-registration/antimicrobial-performance-evaluation-program-apep
4. Rutala WA and Weber DJ. (2014). Selection of the Ideal Disinfectant. ICHE; Vol 35(7).
5. Centers for Disease Control and Prevention. Disinfection and Sterilization, 2008. [Internet]. [Cited 2021, Dec 29]. Available from https://www.cdc.gov/infectioncontrol/guidelines/disinfection/index.html
6. Sassi H, Sifuentes L, Koenig D, Nichols E, Clark-Greuel J, Wong L, et al. Control of the spread of viruses in a long-term care facility using hygiene protocols. AJIC. 2015 Jul 1;43(7):702-6.^














